Overview of Breast Cancer
Statistical Insights and Epidemiological Trends

Breast cancer ranks as the most common cancer among women worldwide, with approximately 23 lakhs new cases diagnosed each year.
Incidence rates vary geographically, with higher rates observed in developed countries compared to developing regions.
Mortality rates from breast cancer have been declining in many high-income countries due to advancements in early detection and treatment, but disparities persist in low- and middle-income countries.
The incidence of breast cancer varies across different regions, with an estimated 90.0 cases per 1,00,000 women globally. Prevalence rates reflect the total number of existing cases at a given time and are influenced by factors such as population demographics and healthcare access. Mortality rates from breast cancer, while decreasing in some regions, remain a significant concern, particularly in areas with limited access to screening and treatment.
Survival rates for breast cancer vary depending on several factors, including stage at diagnosis, tumor characteristics, treatment modalities, and access to healthcare services. Five-year survival rates for breast cancer range from approximately 90% for localized (early-stage) disease to around 27% for metastatic (advanced-stage) disease. Prognostic factors such as hormone receptor status (estrogen receptor, progesterone receptor), HER2/neu expression, tumor grade, and lymph node involvement influence survival outcomes and guide treatment decisions.
Understanding Breast Cancer Types
Breast cancer encompasses a diverse range of subtypes, each with unique characteristics and treatment implications. Understanding these subtypes is crucial for accurate diagnosis and personalized treatment planning.
DCIS is a non-invasive form of breast cancer that originates in the milk ducts. It is characterized by the abnormal growth of cells within the ducts, without invading surrounding tissue. While DCIS is considered a pre-invasive stage of breast cancer, it has the potential to progress to invasive breast cancer if left untreated. Treatment options for DCIS may include surgery, radiation therapy, and hormone therapy, depending on the individual patient's risk factors and preferences.
ILC is a less common subtype of invasive breast cancer, accounting for approximately 10-15% of cases. It originates in the lobules of the breast and tends to spread more diffusely within the breast tissue, making it challenging to detect on imaging studies. ILC may present with subtle symptoms, such as thickening or swelling of the breast, rather than a distinct lump. Treatment for ILC is similar to IDC and may include surgery, radiation therapy, hormone therapy, or targeted therapy, depending on the tumor's characteristics and stage.
IBC is a rare and aggressive form of breast cancer characterized by rapid progression and inflammatory changes in the breast tissue. It typically presents with symptoms such as redness, swelling, warmth, and thickening of the skin, resembling an infection or inflammation. IBC is often diagnosed at an advanced stage and requires aggressive multimodal treatment, including chemotherapy, surgery, radiation therapy, and targeted therapy. Despite its aggressive nature, advances in treatment have improved outcomes for some patients with IBC.
Symptoms of Breast Cancer
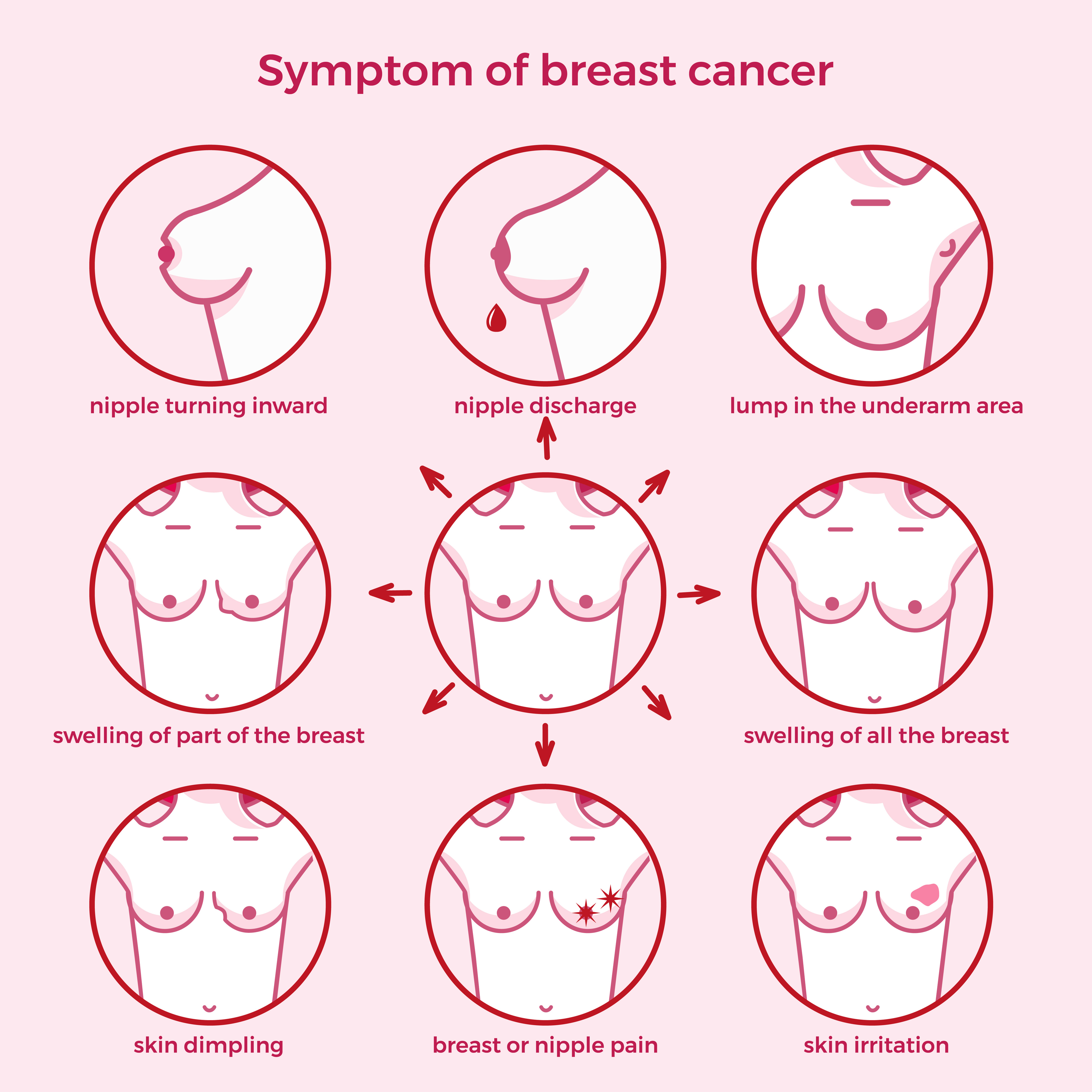
Early detection of breast cancer is essential for timely intervention and improved treatment outcomes. Recognizing the signs and symptoms of breast cancer can facilitate early diagnosis and appropriate management.
Any concerning changes in breast health should prompt a visit to a healthcare provider for further evaluation and management. Early detection of breast cancer improves treatment outcomes and patient survival rates.Schedule an Appointment
Causes and Risk Factors of Breast Cancer
Breast cancer is a complex disease with multifactorial causes and risk factors. Understanding these factors is crucial for identifying individuals at increased risk and implementing appropriate risk-reduction strategies.
Here are the main causes and risk factors of breast cancer
Breast cancer risk factors encompass a range of genetic, hormonal, environmental, and lifestyle influences. One significant risk factor is a family history of breast cancer, particularly among first-degree relatives (such as a mother, sister, or daughter). Individuals with a family history have a higher risk of developing breast cancer compared to those without such history. For instance, women with one first-degree relative diagnosed with breast cancer have approximately twice the risk of developing the disease themselves, while those with multiple affected relatives have an even higher risk.
Moreover, certain genetic mutations, such as BRCA1 and BRCA2 mutations, substantially elevate breast cancer risk. BRCA1 mutation carriers have a lifetime risk of breast cancer ranging from 55% to 65%, while BRCA2 mutation carriers have a risk of 45%. These mutations also increase the risk of other cancers, including ovarian cancer.
For individuals testing positive for BRCA mutations, options for risk reduction and prevention include increased surveillance, risk-reducing surgeries, and chemoprevention (using medications such as tamoxifen or raloxifene). Angelina Jolie's public revelation of her BRCA-positive status and subsequent preventive double mastectomy and oophorectomy have highlighted the importance of genetic testing and risk-reducing interventions for high-risk individuals, sparking widespread awareness and discussion about breast cancer prevention strategies.
Prevention of Breast Cancer
Breast cancer risk factors encompass a range of genetic, hormonal, environmental, and lifestyle influences. One significant risk factor is a family history of breast cancer, particularly among first-degree relatives (such as a mother, sister, or daughter). Individuals with a family history have a higher risk of developing breast cancer compared to those without such history. For instance, women with one first-degree relative diagnosed with breast cancer have approximately twice the risk of developing the disease themselves, while those with multiple affected relatives have an even higher risk.
Diagnosis of Breast Cancer
The diagnosis of breast cancer is a meticulous process involving various diagnostic modalities aimed at confirming the presence of cancer and determining its characteristics. A comprehensive evaluation typically includes:
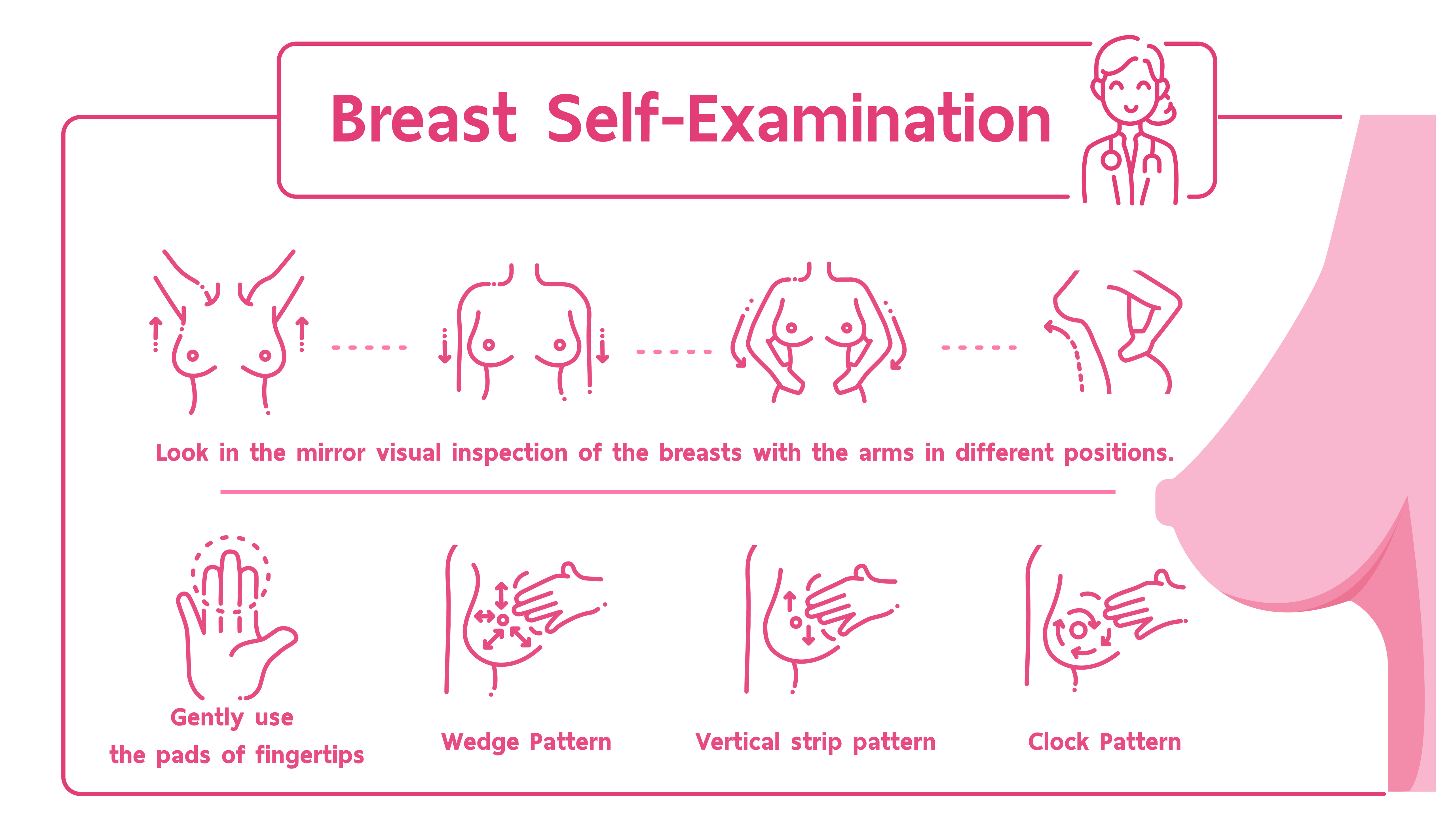
Breast exam
During a clinical breast exam, a healthcare professional looks at the breasts for anything that's not typical. This might include changes in the skin or to the nipple. Then the health professional feels the breasts for lumps. The health professional also feels along the collarbones and around the armpits for lumps.
Mammogram
A mammogram is an X-ray of the breast tissue. Mammograms are commonly used to screen for breast cancer. If a screening mammogram finds something concerning, you might have another mammogram to look at the area more closely. This more-detailed mammogram is called a diagnostic mammogram. It's often used to look closely at both breasts.
Breast ultrasound
Ultrasound uses sound waves to make pictures of structures inside the body. A breast ultrasound may give your healthcare team more information about a breast lump. For example, an ultrasound might show whether the lump is a solid mass or a fluid-filled cyst. The healthcare team uses this information to decide what tests you might need next.
Breast MRI
MRI machines use a magnetic field and radio waves to create pictures of the inside of the body. A breast MRI can make more-detailed pictures of the breast. Sometimes this method is used to look closely for any other areas of cancer in the affected breast. It also might be used to look for cancer in the other breast. Before a breast MRI, you usually receive an injection of dye. The dye helps the tissue show up better in the images.
Removing a sample of breast cells for testing
A biopsy is a procedure to remove a sample of tissue for testing in a lab. To get the sample, a healthcare professional puts a needle through the skin and into the breast tissue. The health professional guides the needle using images created with X-rays, ultrasound or another type of imaging. Once the needle reaches the right place, the health professional uses the needle to draw out tissue from the breast. Often, a marker is placed in the spot where the tissue sample was removed. The small metal marker will show up on imaging tests. The marker helps your healthcare team monitor the area of concern.
Testing cells in the lab
The tissue sample from a biopsy goes to a lab for testing. Tests can show whether the cells in the sample are cancerous. Other tests give information about the type of cancer and how quickly it's growing. Special tests give more details about the cancer cells. For example, tests might look for hormone receptors on the surface of the cells. Your healthcare team uses the results from these tests to make a treatment plan.
Staging breast cancer
Once your healthcare team diagnoses your breast cancer, you may have other tests to figure out the extent of the cancer. This is called the cancer's stage. Your healthcare team uses your cancer's stage to understand your prognosis.
Breast MRI
MRI machines use a magnetic field and radio waves to create pictures of the inside of the body. A breast MRI can make more-detailed pictures of the breast. Sometimes this method is used to look closely for any other areas of cancer in the affected breast. It also might be used to look for cancer in the other breast. Before a breast MRI, you usually receive an injection of dye. The dye helps the tissue show up better in the images.
Complete information about your cancer's stage may not be available until after you undergo breast cancer surgery.
Tests and procedures used to stage breast cancer may include:
Not everyone needs all of these tests. Your healthcare team picks the right tests based on your specific situation.
Breast cancer stages range from 0 to 4. A lower number means the cancer is less advanced and more likely to be cured. Stage 0 breast cancer is cancer that is contained within a breast duct. It hasn't broken out to invade the breast tissue yet. As the cancer grows into the breast tissue and gets more advanced, the stages get higher. A stage 4 breast cancer means that the cancer has spread to other parts of the body.
Treatment
Breast cancer surgery
Lumpectomy
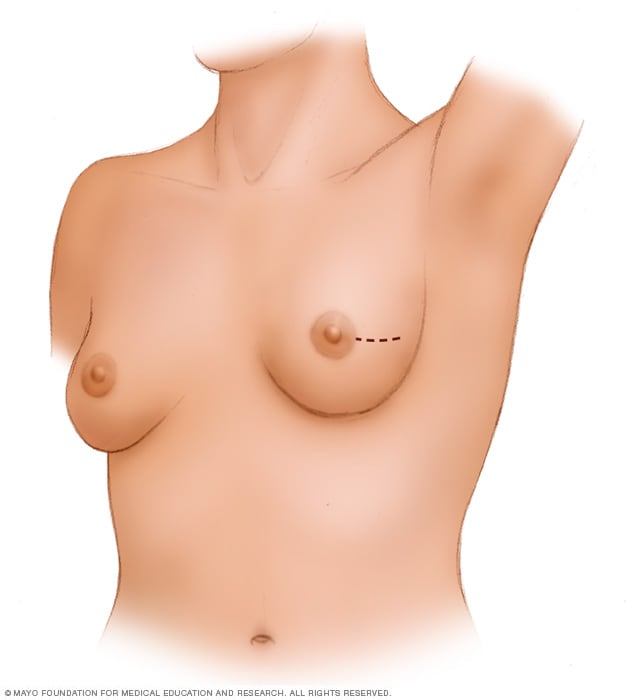
A lumpectomy involves removing the cancer and some of the healthy tissue that surrounds it. This illustration shows one possible incision that can be used for this procedure, though your surgeon will determine the approach that's best for your particular situation.
Mastectomy
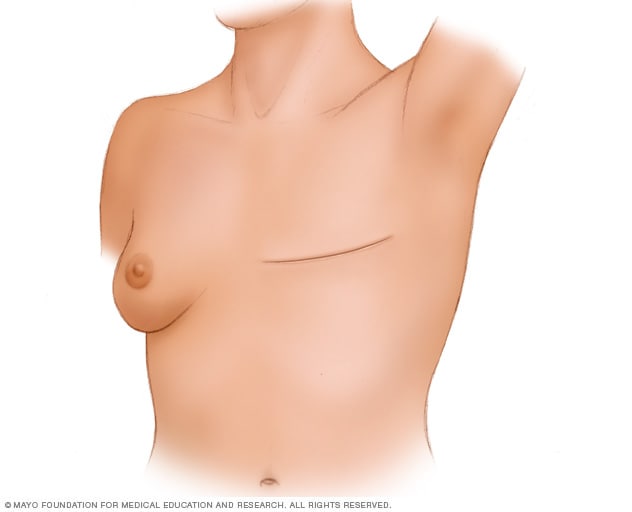
During a total mastectomy, the surgeon removes the breast tissue, nipple, areola and skin. This procedure also is known as a simple mastectomy. Other mastectomy procedures may leave some parts of the breast, such as the skin or the nipple. Surgery to create a new breast is optional.
Sentinel node biopsy
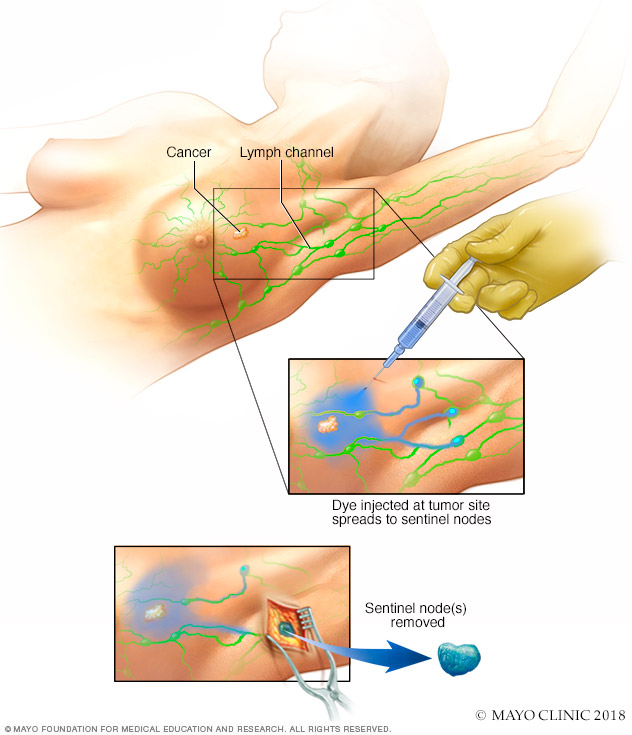
Sentinel node biopsy identifies the first few lymph nodes into which a tumor drains. The surgeon uses a harmless dye and a weak radioactive solution to locate the sentinel nodes. The nodes are removed and tested for signs of cancer.
Radiation therapy
Radiation therapy treats cancer with powerful energy beams. The energy can come from X-rays, protons or other sources.
For breast cancer treatment, the radiation is often external beam radiation. During this type of radiation therapy, you lie on a table while a machine moves around you. The machine directs radiation to precise points on your body. Less often, the radiation can be placed inside the body. This type of radiation is called brachytherapy.
Radiation therapy is often used after surgery. It can kill any cancer cells that might be left after surgery. The radiation lowers the risk of the cancer coming back.
Side effects of radiation therapy include feeling very tired and having a sunburn-like rash where the radiation is aimed. Breast tissue also may look swollen or feel more firm. Rarely, more-serious problems can happen. These include damage to the heart or lungs. Very rarely, a new cancer can grow in the treated area.
Chemotherapy
Chemotherapy involves the use of cytotoxic medications to destroy cancer cells and prevent their growth and spread. It may be administered before surgery (neoadjuvant therapy) to shrink the tumor, after surgery to eradicate any remaining cancer cells (adjuvant therapy), or as a primary treatment modality for advanced-stage or metastatic breast cancer.
Know MoreHormone Therapy
Hormone therapy, also known as endocrine therapy, is used to treat hormone receptor-positive breast cancer by blocking the effects of estrogen or reducing its production in the body. Medications such as tamoxifen, aromatase inhibitors (e.g., letrozole, anastrozole), and selective estrogen receptor modulators (SERMs) are commonly used in hormone therapy.
Know MoreTargeted Therapy
Targeted therapy specifically targets molecular pathways involved in cancer growth and progression. For example, HER2-targeted therapies, such as trastuzumab (Herceptin) and pertuzumab (Perjeta), are used to treat HER2-positive breast cancer. Additionally, CDK4/6 inhibitors, such as palbociclib and ribociclib, are used in combination with hormone therapy for certain hormone receptor-positive breast cancers.
Know MoreImmuno Therapy
Immunotherapy harnesses the body's immune system to recognize and attack cancer cells. While still being researched for breast cancer treatment, immunotherapy has shown promising results, particularly in certain subtypes of breast cancer, such as triple-negative breast cancer (TNBC).
Know MoreScalp Cooling Machine
Chemotherapy-induced alopecia, or hair loss, is a distressing side effect of breast cancer treatment that can significantly impact a patient's self-esteem and quality of life. Scalp cooling machines, such as the Paxman Scalp Cooling System, offer a solution to mitigate this side effect by reducing the risk of hair loss during chemotherapy. By cooling the scalp, these devices constrict blood vessels, limiting the amount of chemotherapy drugs reaching the hair follicles and minimizing hair loss. The availability of scalp cooling machines, such as the Paxman Scalp Cooling System, at Elite Day Care Centre ensures that breast cancer patients undergoing chemotherapy can maintain their hair and improve their comfort and well-being throughout treatment.
Know MorePersonalized Care at Elite Day Care Centre
Elite Day Care Centre is dedicated to providing personalized treatment plans and innovative care for breast cancer patients. Our comprehensive approach integrates advanced technologies, multidisciplinary care teams, and supportive care services to enhance patient outcomes and quality of life. From diagnosis to survivorship, we prioritize individualized care that addresses the unique needs and preferences of each patient, ensuring the best possible treatment experience and outcomes. At Elite Day Care Centre, breast cancer patients can expect compassionate, cutting-edge care that prioritizes their well-being and empowers them throughout their treatment journey.